GLANDS
are cells or aggregations of cells whose function is secretion.
*Exocrine glands: release the secretory product via a system of ducts that opens upon one of the surfaces of the body which are in contact with the external world (skin, gastrointestinal tract etc.).
*Endocrine glands: release their secretory product (typically hormones) into the spaces between the secretory cells (extracellular space) from which it enters the bloodstream.
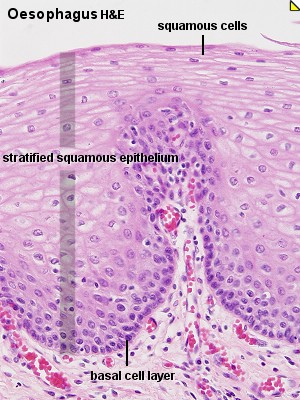
Both endocrine and exocrine glands are developmentally derived from epithelia, which form a down-growth into the underlying connective tissue. The cells forming this down-growth then develop the special characteristics of the mature gland. Exocrine glands maintain the connection with the body surface whereas it is lost by endocrine glands.
--------------------------------------------------------------------------------
*Classification of Exocrine Glands:
Exocrine glands may be classified according to cell number, and/or the shape and branching pattern of their secretory portions and ducts.
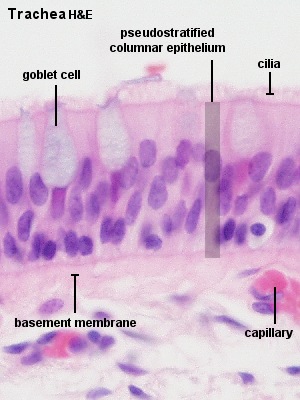
*Unicellular Glands
consist of a single secretory cell. In mammals the only example of unicellular exocrine glands are goblet cells, which occur in the epithelium of many mucous membranes. Goblet cells secrete the glycoprotein mucin, which by the uptake of water is converted into a slimy substance, mucus.
unicellular exocrine glands (goblet cells)
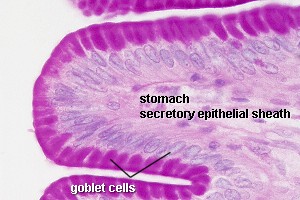
*Multicellular glands :
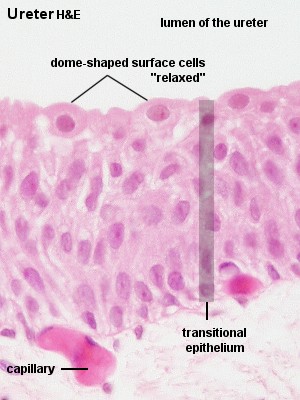
The simplest form of a multicellular gland is a secretory epithelial sheath - a surface epithelium consisting entirely of secretory cells (e.g. the epithelium lining the inner surface of the stomach, where the mucous secretion protects the stomach wall from the acidic contents of the stomach). Other multicellular glands have their secretory portion embedded in the connective tissue underlying the epithelium. The secretion is either discharged directly from the secretory portion onto the epithelium or reaches the epithelium via a duct system that consists of non-secretory cells.
The secretory portion may have a variety of shapes. Secretory cells may form
*tubes in tubular glands,
*acini in acinar glands or
*alveoli in alveolar glands
Combinations exist - the pancreas is a tubulo-acinar gland, in which each section of the secretory system has a specialized function.
The precursors of digestive enzymes are produced by the acinar cells. Tubular cells secrete the alkaline bicarbonate solution which eventually neutralizes the acidic contents of the stomach that are released into the duodenum.
Multicellular glands with an unbranched excretory duct are called simple. We talk about a compound gland when the excretory duct is branched. Finally, the part of the gland consisting of secretory cells is branched in a (surprise!) branched gland.
The classification scheme may appear somewhat elaborate - but there are many exocrine glands around. All of them can be identified and described by this scheme, and some ideas about their function can be derived from this description.
Secretory Mechanisms
The secretory cells can release their secretory products by one of three mechanisms.
1.Merocrine secretion corresponds to the process of exocytosis. Vesicles open onto the surface of the cell, and the secretory product is discharged from the cell without any further loss of cell substance.
2.Apocrine secretion designates a mechanism in which part of the apical cytoplasm of the cells is lost together with the secretory product. The continuity of the plasma membrane is restored by the fusion of the broken edges of the membrane, and the cell is able to accumulate the secretory product anew. This mechanism is used by apocrine sweat glands, the mammary glands and the prostate.
3.Holocrine secretion designates the breakdown and discharge of the entire secretory cell. It is only seen in the sebaceous glands of the skin.
There are two additional mechanisms by which secretory cells can release their products. Lipid soluble substances may diffuse out of the secretory cell (e.g. steroid hormone producing endocrine cells). Transporters (membrane proteins) may actively move the secretory product across the plasma membrane (e.g. the acid producing parietal cells of the gastric glands). These secretory mechanisms may not involve any light microscopically visible specialisations of the cell.
Histological Structure of Large Exocrine Glands:
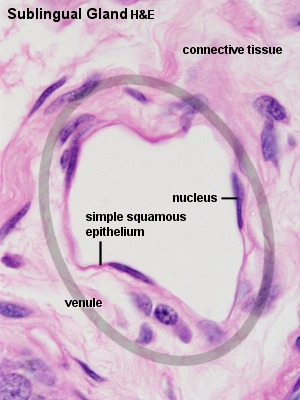
The relationship between the secretory tissue (parenchyma) of glands and the supporting connective tissue is similar in most larger glands. Externally the entire gland is surrounded by a layer of dense connective tissue, the capsule. Connective tissue sheets (septa) extend from the capsule into the secretory tissue and subdivide the gland into a number of lobes. Thinner connective tissue septa subdivide the lobes into a number of lobules. Reticular connective tissue (hardly visible in H&E stained sections) surrounds and supports the secretory units of the glands (alveoli, acini etc.) and the initial parts of the excretory ducts if present.
Blood and lymph vessels as well as nerves penetrate the capsule and form a delicate network between the secretory units and the initial parts of the duct system.
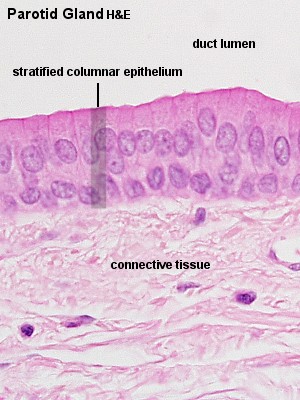
The main excretory duct conveys the secretory product to one of the external surfaces of the body. Other parts of the duct system are named according to their relation to the lobes and lobules of the gland.
*Lobar ducts are are large branches of the main duct which extend to the lobes of the gland. They may be called Interlobar ducts.
*Interlobar ducts if they are found in the connective tissue surrounding the lobes. Interlobar ducts branch and give rise to Interlobular ducts.
*Interlobular ducts, which are found in the connective tissue surrounding the individual lobules of the gland. Branches of the interlobular ducts enter the lobules and are now called Intralobular ducts.
*Intralobular ducts. The terminal branches of the duct system, which connect intralobular ducts with the secretory units of the gland, are called Intercalated ducts.
*Intercalated ducts.
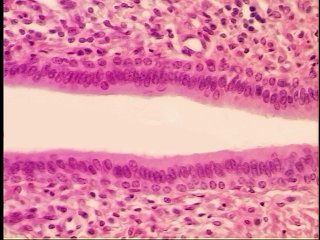
The appearance of the different portions of the duct system is quite variable from gland to gland and may allow the identification of the gland. Quite often, the appearance of parts of the duct system also permits some deductions about their functions.
*Note that lobes and lobules are defined by their relationship to each other. Many small lobules may form one large lobe. Neither size nor the spatial relationship between different parts of the tissue can be unequivocally determined in a single, two-dimensional section of the tissue. Lobes and interlobar ducts may therefore be difficult to distinguish from lobules and interlobular ducts.
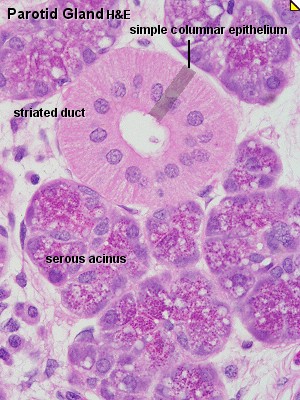
Parotid Gland:alveolar gland
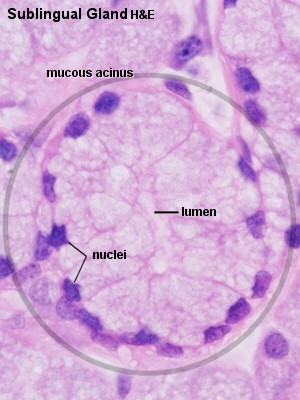
Sublingual Gland:alveolar gland
==============================================================